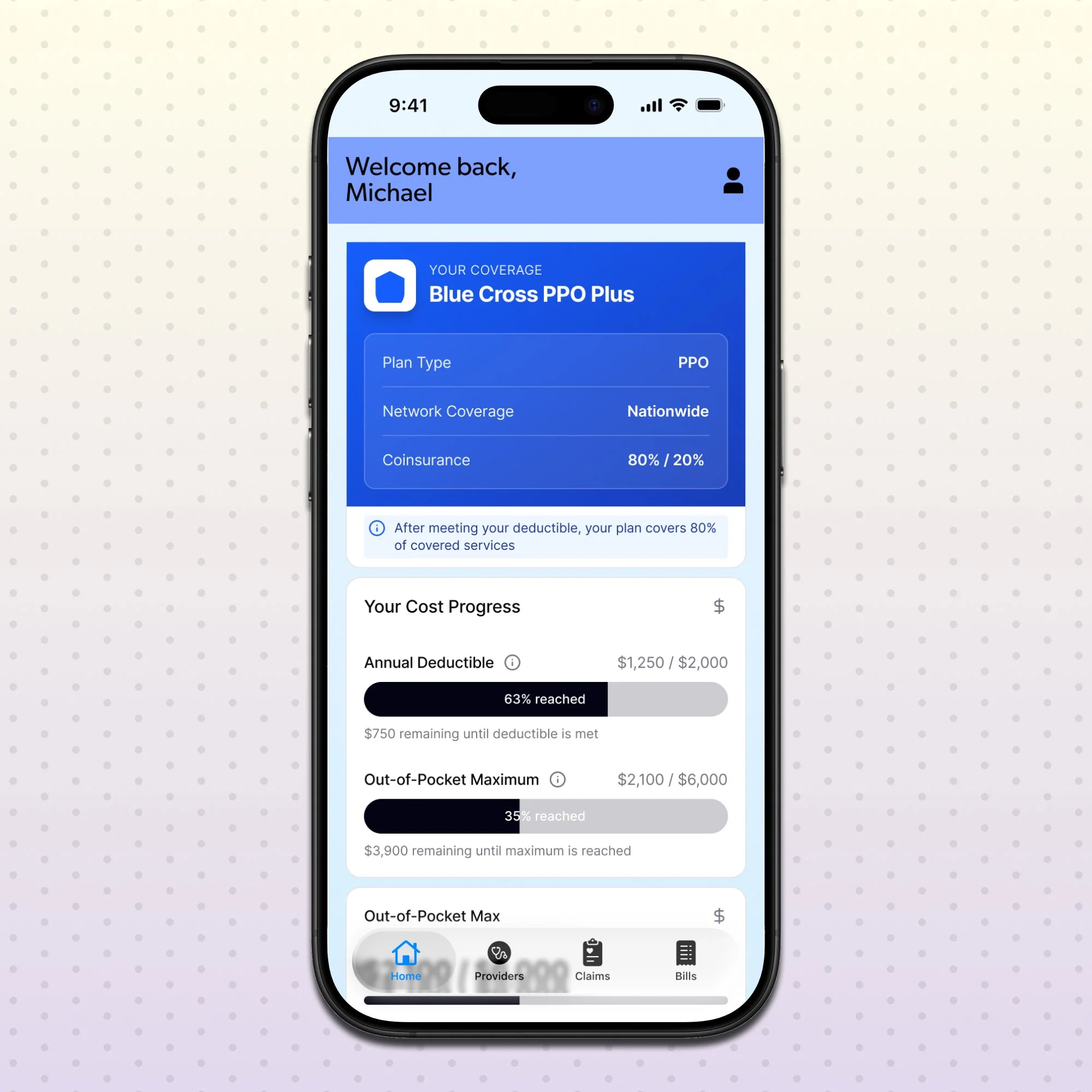
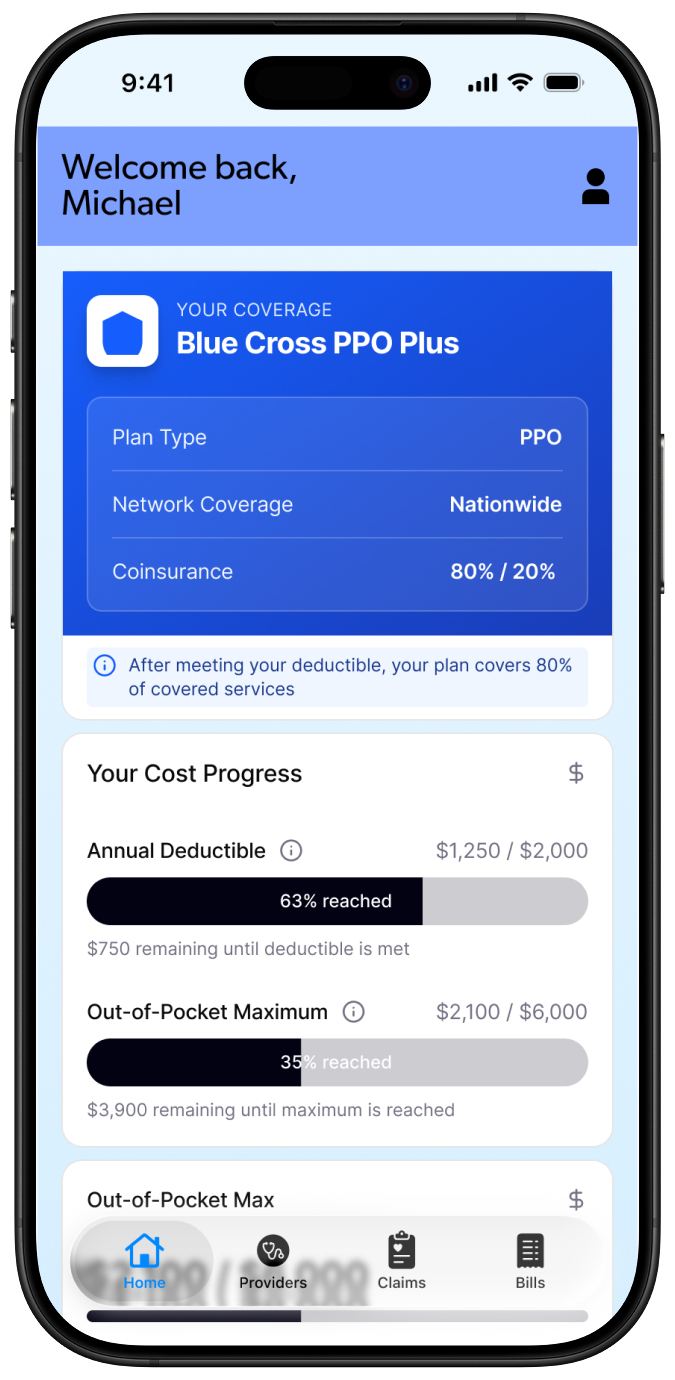
MyHealth App
Bringing clarity, control, and empowerment to healthcare billing and claims.
Project Details
Healthcare billing and insurance claims are often confusing, opaque, and frustrating for patients. Users receive bills with unfamiliar codes, aren’t sure what insurance covers, and struggle to understand why claims are approved or denied. Traditional provider and insurer apps tend to hide key capabilities, like submitting a claim, deep in settings menus or buried workflows.
This product was designed to provide users with a clear, unified view of their healthcare billing and claims, and to surface critical capabilities like claims submission where they are most visible and useful.
Role: Product Designer, UX strategy, user flows, UI design, interaction specification.
The Challenge
Healthcare billing is complex. Confusion costs users time, money, and trust.
Patients often struggle with:
Understanding what they are being billed for
Interpreting insurance adjustments
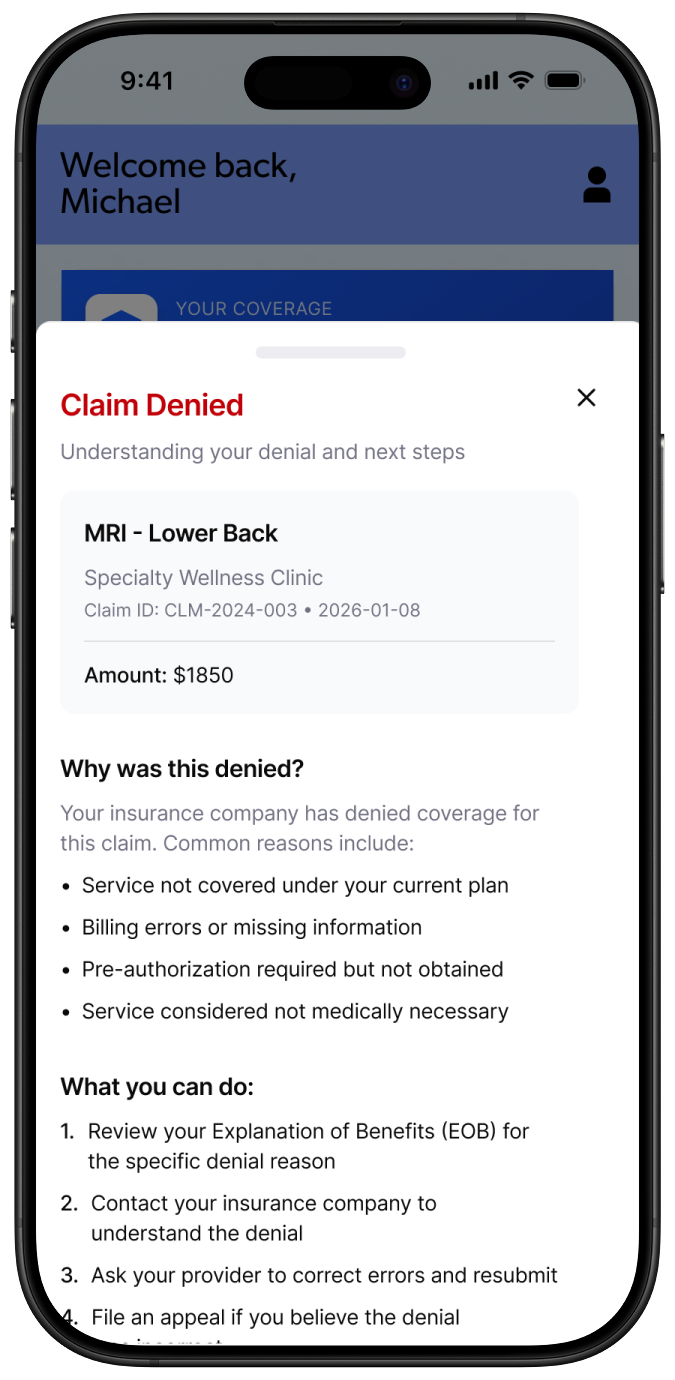
Knowing when a claim is denied or approved and why
Finding and submitting claims forms buried deep in apps
Most existing apps fail to address these needs because:
Billing information is fragmented
Claims tools are hidden or hard to access
Explanations use insurance jargon
Users don’t know what actions they can take next
Research & Discovery
Over my discovery process I was able to validate my assumptions by uncovering key frustration points other users were suffering from.
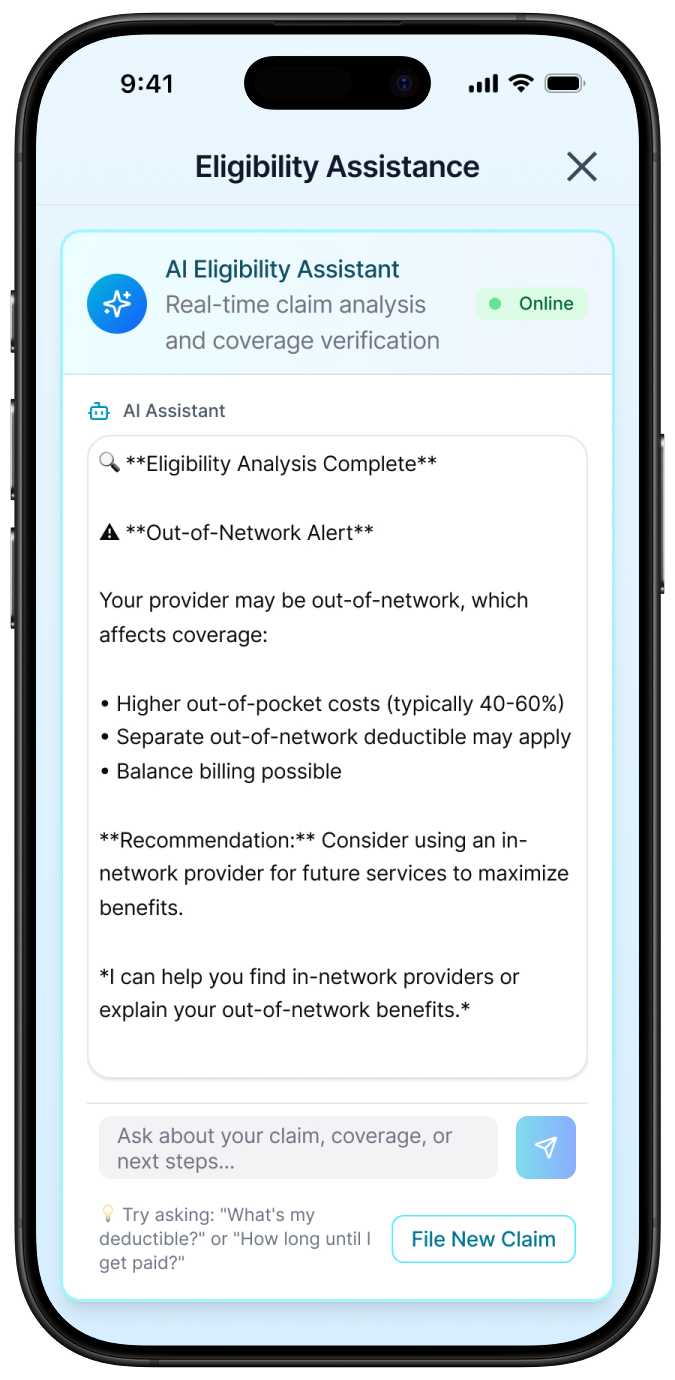
Users don’t read insurance codes — they want plain language explanations.
Claims submission is a pain point — bad discoverability leads to abandonment.
Users want a single dashboard — no more jumping between tabs or menus.
Time to resolution is unclear — users want transparency around expected timelines.
This feedback directly informed my decision making in creating in this application as well. These frustrations mirrored my similar frustrations navigating the healthcare system as I have had similar frustrations or even more.
Key Features Designed
-
Financial totals (outstanding balance, upcoming due)
Recent bills and claims
Alerts (actions required, new statuses)
-
Each bill shows:
Provider charges
Insurance adjustments
Remaining balance
Explanations in plain language
Expandable line items and tooltips help users drill down without overwhelm.
-
Claims have:
Clear status labels (Pending / Approved / Denied)
Timeline of activity
Reason for denial in concise language
Suggested next steps (appeal, contact provider, attach more evidence)
This turns an opaque process into an actionable pathway.
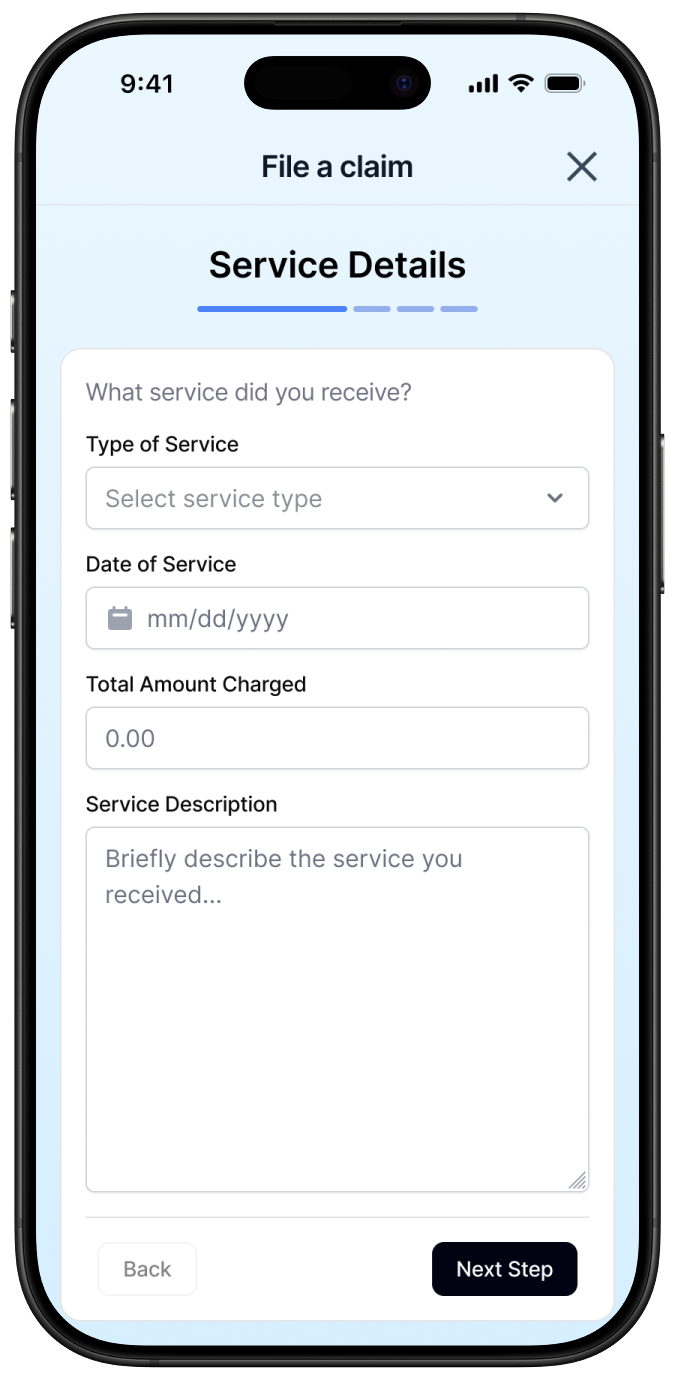
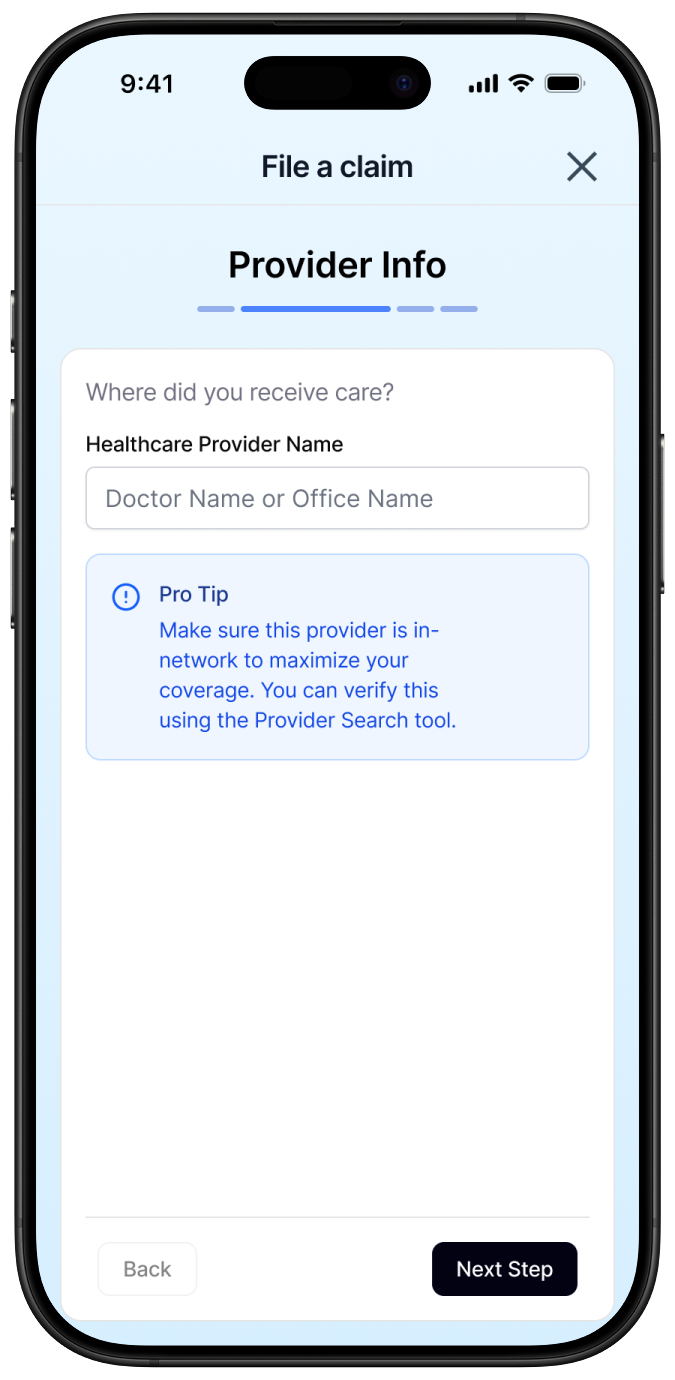
-
Unlike traditional apps, this feature is visible:
From the main dashboard
With a consistent CTA button
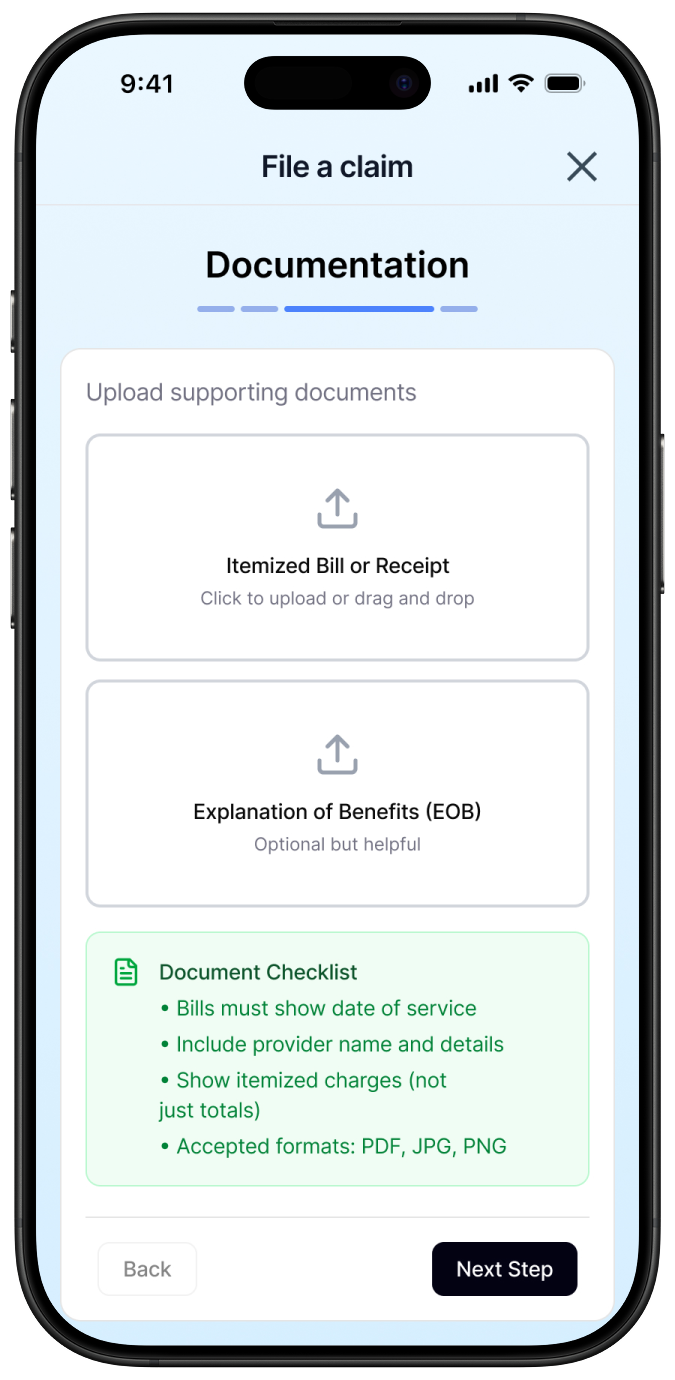
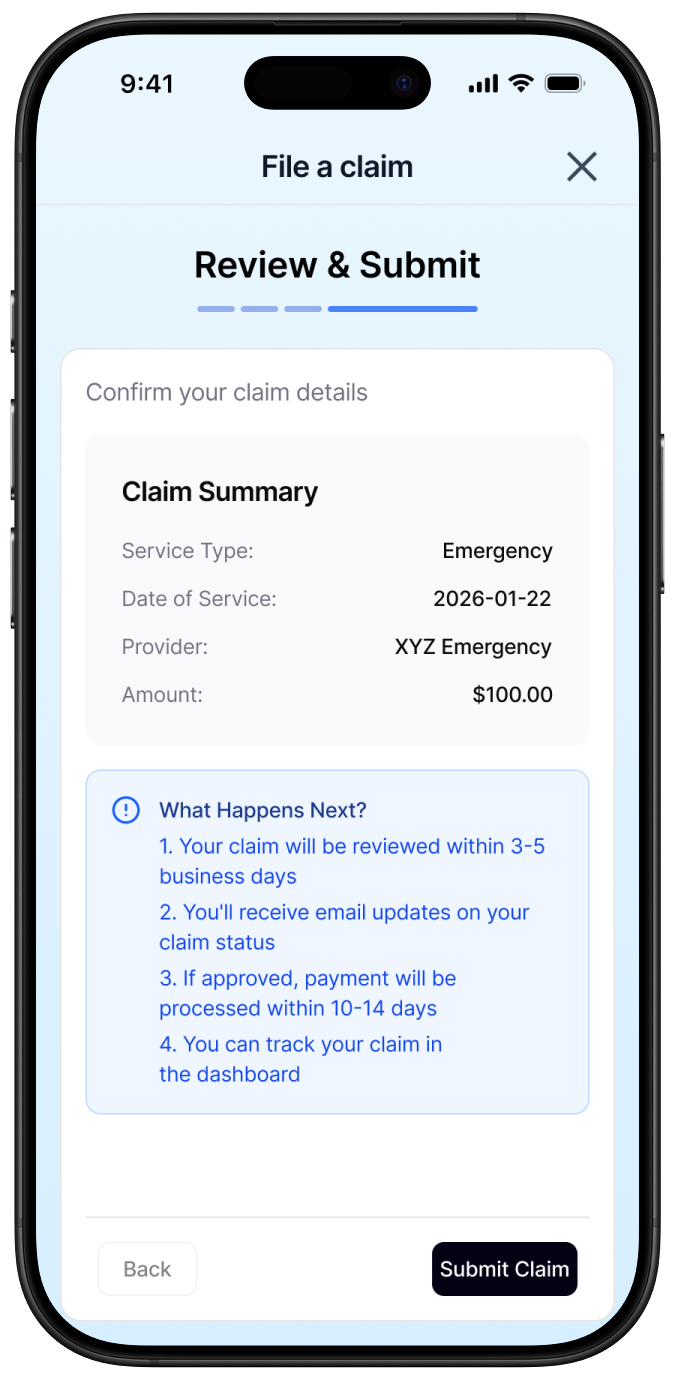
Flow highlights:
Select related bill or service
Pre-filled fields where possible
Attach files/photos
Review & submit
Final Summary
This healthcare billing and claims application flips the typical model on its head by bringing critical workflows to the forefront and making clarity, empowerment, and actionability the heart of the experience. Users get:
Clear explanations of bills
A central dashboard of what matters
A faster, guided path to claim resolution
It’s not just a bill viewer, it’s a billing partner.